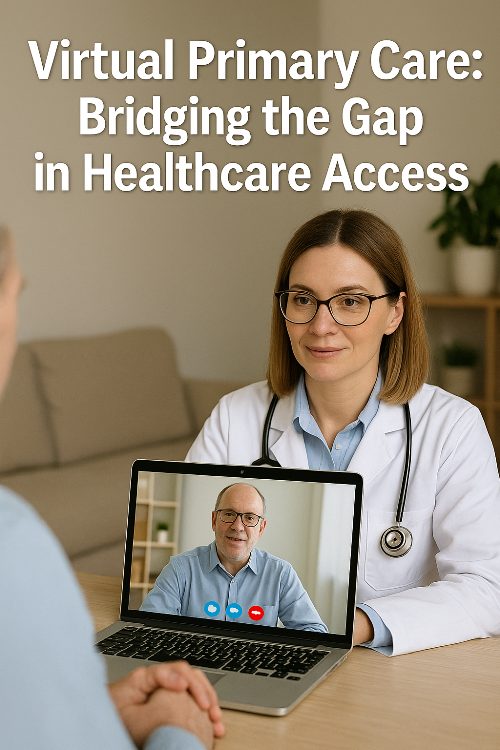
Virtual Primary Care: Bridging the Gap in Healthcare Access
The present-day era is based on convenience, which naturally makes consumers wiser about their purchases. Furthermore, in many parts of the globe, healthcare consumers can now get primary care wherever they are. This is contrary to the traditional brick-and-mortar setup. This digital era is key to removing numerous long-term disadvantages in healthcare implementation while remaining approachable and personal to patients who seek it.
The Growing Need for Accessible Care
In the last few decades, conventional primary care has been met with many problems. There is a deficit of doctors in the US, and appointments are usually challenging, taking many days. In fact, people in rural societies often have to cover long distances to access basic health services. Doctors seem to keep Monday to Friday because there is a huge queue to get diagnosed with many illnesses, which makes busy executives put off much-needed care.
Virtual primary care platforms aim to fill these voids, providing an alternative which dispenses distance and time considerations. Such a strategy is not just applied during this pandemic; it changes how a health system thinks about delivering preventive and routine health care.
Beyond Simple Convenience
While convenience certainly drives adoption, virtual primary care provides benefits that accommodate them beyond scheduling flexibility. The virtual format gives a feeling of closeness that allows the patients to talk easily about matters concerning health which would otherwise have them remarkably uncomfortable and hesitant. With no hassles of traffic, parking and waiting for the room, the time allotted for consultations is spent on the actual health issues rather on the passing nuisances.
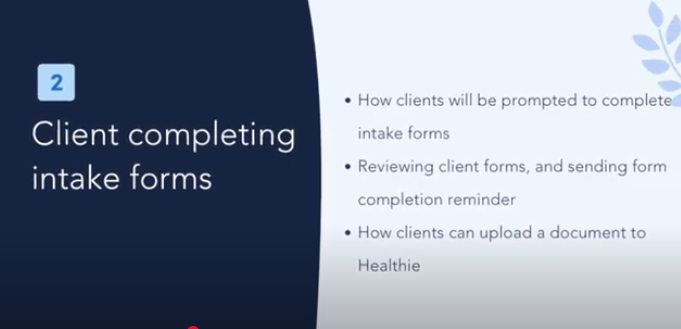
Modern virtual platforms enable seamless integration of health records, prescription management, and follow-up communications—creating a comprehensive ecosystem rather than isolated interactions. This connected approach helps prevent the fragmentation that often undermines effective healthcare delivery.
Maintaining Quality in Virtual Environments
Critics initially questioned whether virtual visits could match the quality of in-person care. However, evidence increasingly shows that virtual primary care can produce comparable outcomes for many common conditions while enhancing patient satisfaction. The key lies in thoughtfully designed platforms facilitating thorough assessment and meaningful provider-patient relationships.
The most effective virtual primary care services employ licensed physicians and nurse practitioners who spend adequate time with each patient, listening carefully to concerns and providing personalized guidance. Many platforms now offer 24/7 availability for urgent needs, combined with consistent access to the same provider for ongoing care—preserving the relational aspect that makes traditional primary care effective.
Complementing Traditional Care
Rather than replacing face-to-face medicine entirely, virtual primary care works best as part of a hybrid approach. Digital platforms excel at managing straightforward conditions, medication management, and preventive counseling. Meanwhile, complex diagnoses, physical examinations, and procedures still require in-person visits.
Forward-thinking providers now offer membership models that allow patients to seamlessly transition between virtual and in-office appointments based on clinical needs. This integrated approach maximises convenience without sacrificing comprehensive care.
The Future Landscape
As technology advances, virtual primary care continues evolving beyond simple video consultations. Remote monitoring tools, AI-assisted screening, and secure messaging create continuous connections between patients and providers rather than episodic interactions. With mounting evidence supporting clinical effectiveness and patient preference, virtual primary care is positioned to become a fundamental component of modern healthcare delivery. By removing barriers to access while maintaining personalised attention, this model promises to help more Americans engage with preventive care and manage chronic conditions effectively—potentially improving outcomes while reducing overall healthcare costs.